Vaginoplasty
Gender Confirmation Surgery
Medically reviewed by Tuan A. Tran, M.D., M.B.A., F.A.C.S. | Written by Nhuhao Do on May 27th, 2021
Overview
Transgender and intersex people follow different paths to express their gender identity. Some may choose to pursue gender confirmation surgery (GCS), also known as sex reassignment surgery (SRS) or bottom surgery to better identify with their gender expression. This article will focus on bottom surgery for assigned male at birth (AMAB). Male-to-female, or male to non-binary people may elect to undergo vaginoplasty to obtain female genital. They may also decide to pursue other procedures as part of gender confirmation surgery including, chest reconstruction and facial feminization surgery.
Before the surgery
A good candidate for vaginoplasty is a healthy adult with realistic expectations of what the procedure can help them achieve along with the understanding of potential risks. Before proceeding with your surgery, your surgeon will go over an informed consent with you; you will be asked to provide a psychiatric evaluation; and other medical screening including, blood tests and electrocardiogram (EKG).
Leading up to your surgery, you will be required to stop hormone replacement therapy (HRT) for two weeks before surgery, and refrain for another two weeks after surgery. Most people will also need to go through hair removal via electrolysis. In vaginoplasty, hair will be removed on the skin that will eventually comprise the lining of the neovagina. Be sure to discuss in detail with Dr. Tran about the any medications that you take regularly and any recreational drugs you may use. He will advise whether or not you will need to stop taking any of those medications before your surgery.
Procedure in Detail
There are three main methods of vaginoplasty performed today:
- Penile inversion
- Rectosigmoid or colon graft
- Non-penile inversion vaginoplasty
In all three surgical methods, the clitoris is sculpted from the head of the penis. Dr. Tran will discuss with you to determine the best technique for body to achieve your desired results.
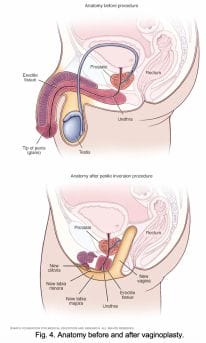
Penile inversion
Penile inversion involves using the penile skin to form the neovagina. The labia major and minora are primarily made from scrotal tissue. This results in a sensate vagina and labia.
One main drawback is the lack of self-lubrication by the vaginal wall. Common variations include using the remaining scrotal tissue as a graft for additional vaginal depth, and using the intact mucosal urethra recovered from the penis to line part of the vagina, creating some self-lubrication.
Rectosigmoid vaginoplasty
Rectosigmoid vaginoplasty involves the use of intestinal tissue to form the vaginal wall. This technique is sometimes used in conjunction with penile inversion. Intestinal tissue helps when penile and scrotal tissue is scarce.
This method is an option for transgender women who began hormone therapy at puberty and were never exposed to testosterone.
Intestinal tissue offers the benefit of being mucosal, and therefore self-lubricating. This technique is also used to reconstruct vaginas for cisgender women who developed atypically short vaginal canals.
Non-penile inversion
Non-penile inversion is also known as the Suporn technique or the Chonburi Flap. This method uses perforated scrotal tissue graft for the vaginal lining, and intact scrotal tissue for the labia majora similar to the penile inversion technique. The penile tissue is used for the labia minora and clitoral hood. This technique reported greater vaginal depth, more sensate inner labia, and improved cosmetic appearance.
Recovery
After your surgery, you will stay hospitalized for 3-6 days. During that time, you will have a catheter until you can purge the bulk of your urine through your urethra on your own. You will follow-up with Dr. Tran 7 days after your surgery for a post-operative appointment.
Risks and side effects
Pain and swelling are expected after your surgery. Some may experience minor urinary incontinence, similar to that after giving birth and should subsides overtime. Although rare, there are other side effects after vaginoplasty to be considered:
- Loss of sensation in part or all of the neoclitoris due to nerve damage
- Rectovaginal fistula
- Vaginal prolapse
Cost and Consultation
Many major medical insurances in California, including CalOptima, cover for vaginoplasty as part of gender confirmation surgery. If you have more questions or would like to schedule a free consultation with Dr. Tran, please contact us via our website, Tran Plastic mobile app or call us today at 714-839-8000.
References
Bizic M., Kojovic, V., Duisin, D., Stanojecvic, D., Vujovic, S., Milosevic, A., Korac, G., & Djordjevic, M. (2014, May 26). An overview of neovaginal reconstruction options in male to female transsexuals. Hindawi The Scientific World Journal. DOI: dx.doi.org/10.1155/2014/638919
Cavanaugh, T., Hopwood, R., & Lambert, C. (2016, November 18). Informed consent in the medical care of transgender and gender-nonconforming patients. AMA Journal of Ethics | Illuminating the Art of Medicine. Retreived from journalofethics.ama-assn.org/2016/11/sect1-1611.html
Mayo Clinic Staff. Anatomy before and after penile inversion. Mayo Clinic. Mayo Clinic. Retrieved from https://www.mayoclinic.org/tests-procedures/feminizing-surgery/multimedia/img-20358606
Watanyusakul, S. (2002, July 27). A new method for sensated clitoris and labia minora reconstruction in male-to-female sex reassignment surgery. Aikchol Hospital, Chonburi. Retrieved from https://supornclinic.com/paper/
Weyers, S., Verstraelen, H., Gerris, J., Monstrey, S., Santiago, G., Saerens, B., Backer, E., Claeys, G., Vaneechoutte, M., & Verhelst, R. (2009, May 20). Microflora of the penile skin-lined neovagina in